After COVID-19
COVID-19 isn’t just changing what we do today, it along with however it may mutate in the future is very likely to change how we arrange, manage and administer our businesses for years into the future. And with recent reports postulating that the hoped-for herd immunity may not occur, dependence on both vaccine and therapeutics may become a regular part of our medical care.
What then does this mean for restarting your hospital or medical staff? First, it means a return to 2019 normal simply will not occur. Second, it means you have many, many decisions to make regarding changes in market demand, changes in reimbursement, changes in risk, changes in staffing, changes in use of technology, changes in facility deployment, changes in supply (PPE) management and changes at an administrative leadership level.
Today, walking into a patient waiting area, it’s common to see every other chair taped off as a means of encouraging social distancing. It’s also common to see signs requiring face masks. It’s also, unfortunately, not uncommon to see people sitting in those taped off chairs and people not wearing masks. So, as you look at all the changes to be considered, consider also, the volatile nature of changes in personal, social responsibility.
Watching the news, we can readily see what happens when public compliance is relied on – conflict in mayhem. We can also see what happens when businesses accept personal, social responsibility enforcement as their responsibility – opportunities to enhance the customer experience and create a safer environment for everyone.
So, what will be your response? Do you have a steering committee established to address these myriad issues and to chart a course for business success in the new 21st century, or is “hope” your strategy… hope that something miraculous will occur and it will be 2019 again?
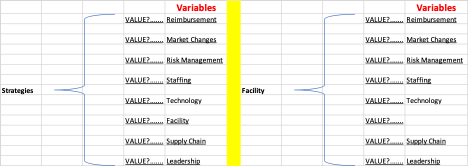
If your strategy is proaction versus hope, then the next step beyond establishing a leadership group to address these issues is to collect and construct data in order to derive the definition of successful strategies. Again, the choice is yours: data driven decisions or gut-driven decisions. And, we’ve seen for the past six months what happens when “gut” instincts rather than empirical data is used to make decisions. Assuming you want to follow the data, consider the analytical structure in Figure 1.
This is based on a Markov model focused on Cost Effectiveness Analysis. Overall, the objective is to derive specific strategies for all areas of operational review. The left chart represents the overall objective, that is the valuation and definition of input variable to output a strategy. The right-hand table represents the selection of one such strategy area, “facilities,” and positions it as the strategy focus. Then, values may be assigned to the other Variables that have an impact on the Facility Strategy. This represents the proverbial 30,000-foot view. Functionally, for example, sub-charts would be constructed to illustrate the various staff involved in facility operations. This would range from housekeeping to administrative leadership and each tier in between. The same would or could be true for Risk Management, as Risk is both an internal and an external factor. The point is this. This level of analysis provides the leadership team with objectively derived actionable data for much more effective decision-making than typical consultant or committee driven initiatives.
Figure 1.